The Mystery of Modern Medicine
As Einstein said "The most beautiful thing we can experience is the mysterious. It is the source of all true art and all science."
In a previous post, I said that “modern medicine aspires to be a body of scientifically validated knowledge and techniques, resting on a solid foundation of basic sciences.”
I chose the word “aspires” carefully. To aspire is to hope to achieve something. It assumes an attainable and desirable target.
As it stands, our scientific knowledge remains incomplete. Not all of our current knowledge and techniques are scientifically validated, nor is the basic science foundation as solid as some believe. Indeed, the more we learn, the more we come to appreciate the gaps in our knowledge.
Indeed, unless you believe that everything about humans and their pathology is ultimately knowable and predictable, then medicine can never be a purely (or entirely) scientific pursuit, like mathematics, physics, or chemistry.
Closing the gaps in our knowledge may not be attainable, or desirable.
Realistically, medicine is more of an applied science, like engineering or architecture, where scientific tools and concepts are used judiciously to suggest various possible solutions for specific problems, accepting that no two problems are exactly alike.
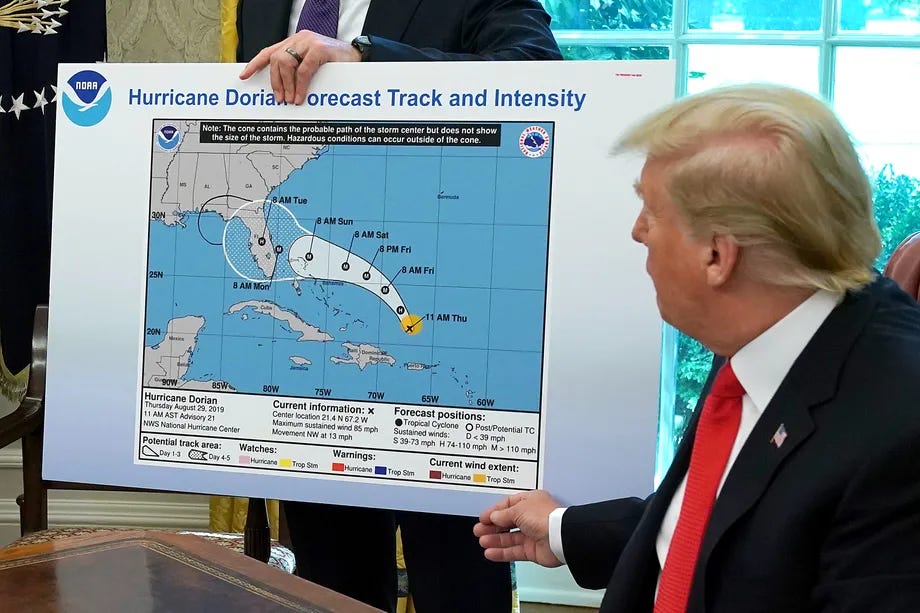
As an example, consider another applied science, weather forecasting. Individual weather events are unique, but they do fall into broad categories, ranging from heat waves to pleasant days through rain storms to hurricanes and blizzards. As our meteorological observations have become more detailed over the years, we understand weather events better. Weather forecasting has improved, but we all know that it’s not 100% accurate, nor will it ever be. At best, weather forecasts describe the probability of certain events over short time frames in certain broad geographic areas. For instance, we can say when conditions are ripe for tornadoes, but we can’t say for certain when, where or even if they will appear. For any weather event, the uncertainty increases as you look at specific communities or longer time frames, approaching the level of fiction when you see articles describing what kind of winter it’s likely to be.
As with weather events, all people are unique. Even though their diseases fall into broadly similar categories, their illness experiences are also unique, even more so when you consider individual values and preferences. Uncertainty and complexity are facts of life. Because medical science derives its evidence from the average experiences of groups of people, it is by definition “medicine-in-general”, even though some very smart doctors purport to provide “precision” medicine or threaten “unavoidable” future consequences based on current behaviours, like smoking. Yes, we can describe which groups of people are at greater risk of heart attacks, including smokers. However, we can never be certain that any individual smoker will actually have a heart attack or that his non-smoking twin won’t.
Individual clinical advice and decisions can never be 100% certain and will always reflect the probabilities of various explanations and outcomes, particularly over the longer term. As such, there will always be room for clinical judgment. Translating general medical knowledge to the personalized care of the individual patient is the art (or heart) of medicine, and it will never be perfect.
Let’s consider this in greater depth.
There are three types of systems; simple, complicated, and complex.
Consider the flashlight, a simple system involving a battery, a switch and a light bulb, all linked together with wires and enclosed in a case. The parts are standard and interchangeable. When you flip the switch, it lights up; it’s predictable (the fancy word is “deterministic”). The surroundings don’t matter; you’ll get the same result regardless of where it was made or where you are when you turn it on. There are only so many ways it can fail. Either the light bulb has burned out, the switch is broken, the wires are disconnected, or the battery is dead. The flashlight won’t fix itself, but repairing the defect immediately puts the system back in working order.
Complicated systems consist of multiple simple systems working together. In a car, for example, thousands of components are organized into various systems, some more complicated than others, including the engine, the drivetrain, the suspension, the seats, etc. The systems interact in knowable and specific ways. The parts are all standardized and interchangeable; they can each be measured and described in detail, as can the entire assembly. If you pull two identical cars apart, mix the parts, and then reassemble them, you’ll still have two identical cars. Studying all the parts and their interactions allows you to accurately predict how the entire system operates. Any one of the components or subsystems could go wrong, rendering the entire car useless. However, the potential failure points, numerous as they are, can all be identified. Repair manuals exist. The car won’t fix itself, but once the mechanic works their magic, the car runs as before. Cars don’t benefit from experience. Driving through icy conditions while carrying heavy goods doesn’t make the car smarter or stronger. In the end, cars are reliable, predictable, reproducible, and fixable.
People are not simple or complicated. People are complex.
Traffic is also complex. It’s not predictable, it’s “probabilistic”. No matter how much you study the drivers, vehicles, roads, intersections, etc. and all their interactions, you will never be able to accurately predict how the entire road system will operate at any given time. The whole is greater than the sum of the parts. You can estimate when and where the traffic jams are likely to be found, but you will be wrong at times, in part because traffic is “nonlinear”, meaning that there’s no direct proportional relationship between an event and its consequences. A trivial fender bender can cause gridlock, while an overturned car in the ditch can go unnoticed for days. A huge new intersection might simply move the traffic jam down the road, while a minor adjustment in a traffic light can a big difference. Traffic adapts; when there’s a problem, detours are put in place, drivers find new routes and modify their habits, and new patterns are established.
Dating back to the 1600’s, medicine has followed a reductionist path, looking into the human body as if it were a machine, studying all the parts and their interactions to see how the entire system operates. Anatomical dissection allowed us to look inside the dead and surgical dissection inside the living. Powerful imaging tools (first xrays then CT scans and now MRI scans) let us look inside, without the need to cut. Through optical microscopes and then electron microscopes, we saw inside tissues and cells, both healthy and diseased. Biochemistry described the chemical processes within cells and organs, while EKGs, EEGs and functional MRI showed their electrical activity. Genetics explored the DNA that specifies our structure and function.
This kind of approach works well with simple and complicated systems but fails miserably when applied to complex systems.
In complexity, you must study the system as a whole rather than focusing on the parts, which interact to create “emergent”, unexpected and unpredictable results. Consider:
Identical twins share their genetic code, but everyone else is genetically unique. We mapped the human genome, only to find that the vast majority of our traits and problems are genetically complex, arising from the actions and interactions of hundreds or even thousands of genes.
No two of us are alike on the outside. Even twins show slight differences. We recognize our friends and family at a glance, precisely because they are unique.
Internally, there are just as many anatomical variations, most of which have no impact on function. Some people are complete mirror images (“situs inversus”), while others are partial mirror images (i.e. dextrocardia, where the heart is on the right rather than the left). Smaller variations often complicate surgery or the interpretation of images, like x-rays. We cannot assume that everyone is the same.
Our parts are not standard, interchangeable, or unchanging. Noses have common features, but it’s impossible to fully define a “normal” nose (or any other body part). We can transplant organs, but then we administer anti-rejection drugs to stop the immune system from rejecting the new non-interchangeable part. Body parts grow, learn and heal over time.
Functionally, we are made up of multiple interdependent systems, none necessarily more important than any other, all of them complex in their own way. You can die of heart disease as easily as you can from kidney disease. On the other hand, sometimes your kidneys save you when your heart runs into trouble.
Behaviourally, two people might react differently to the same event, while individually we can react to the same sort of event differently at different times. There’s no single answer. You can do everything right as a parent and your child might still grow up to be a psychopath.
Our systems are nonlinear. Similar events can trigger very different consequences. Lose a teaspoon of blood from a cut on your finger and you'll probably have to change your Band-Aid. Lose a teaspoon of blood into your brainstem and it might well kill you. A young healthy athlete who breaks their femur could lose a cup or two of blood into the deep tissues of the thigh and not suffer any ill effects from the blood loss itself. A frail elderly person with borderline heart function might well suffer devastating complications from losing even half that amount of blood.
The human body often fixes itself. With or without medical intervention, wounds continue to heal for weeks or months. Some get infected and others fall apart. At other times, our repair mechanisms spin out of control, as with autoimmune conditions like rheumatoid arthritis, where the immune system attacks the joints.
Our systems “learn”. Having seen one variant of the influenza virus, our immune system will be better equipped to respond to future exposures.
I could go on forever! By now, however, it should be obvious that each individual human is unique, unpredictable, “self-organizing”, constantly changing, and affected by their surroundings.
Interestingly (and sadly), even though these complex systems are the very essence of our being, they are rarely mentioned in medical texts.
Our “scientific” understanding of the structure and function of human beings is always going to be based on probabilities, not certainties, even at the most basic level. When dealing with individual people we must adapt to the realities of each specific situation.
Similarly, our understanding of disease is based on observations over hundreds of years and countless people, but it still comes down to probabilities.
There is no blood pressure reading at which you are guaranteed to have a heart attack.
Some features of that melanoma might make it more likely that it will spread to other organs, but we still can’t say with absolute certainty which ones will and which ones won’t.
Randomized controlled trials and “science” cannot specify obligatory actions for any particular patient.
In deciding how to treat your illness and how to apply the general science we know to you as a unique being at this point in time, we’ll have to exercise judgment.
Applying science is an art.



So the whole culture of "shipshape and Bristol fashion", seems to be how to maintain that useful fixable, deterministic quality as you add humans from fishing boat/motor and 1 man crew, up to air craft carrier and 10,000 crew....